Reducing unnecessary conveyances for Frailty patients
Impact
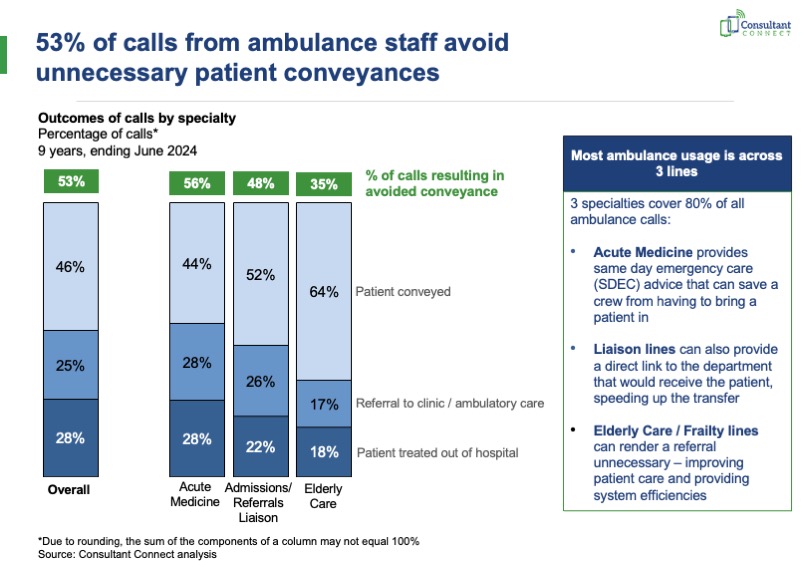
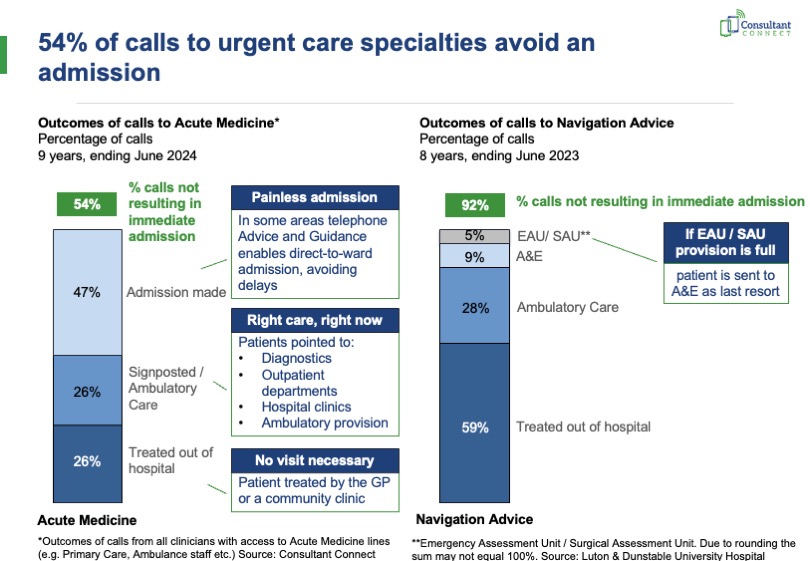
In many instances, an immediate verbal conversation with a Frailty specialist can render a referral or admission unnecessary – improving patient care and providing system efficiencies. Our technology enables that near-instant sharing of such advice and guidance across a variety of pathways.
Learn more about the impact Consultant Connect in our latest Enhanced Advice & Guidance Performance Benchmarks.
Examples in practice
Keeping Frailty patients out of hospital
in South Warwickshire
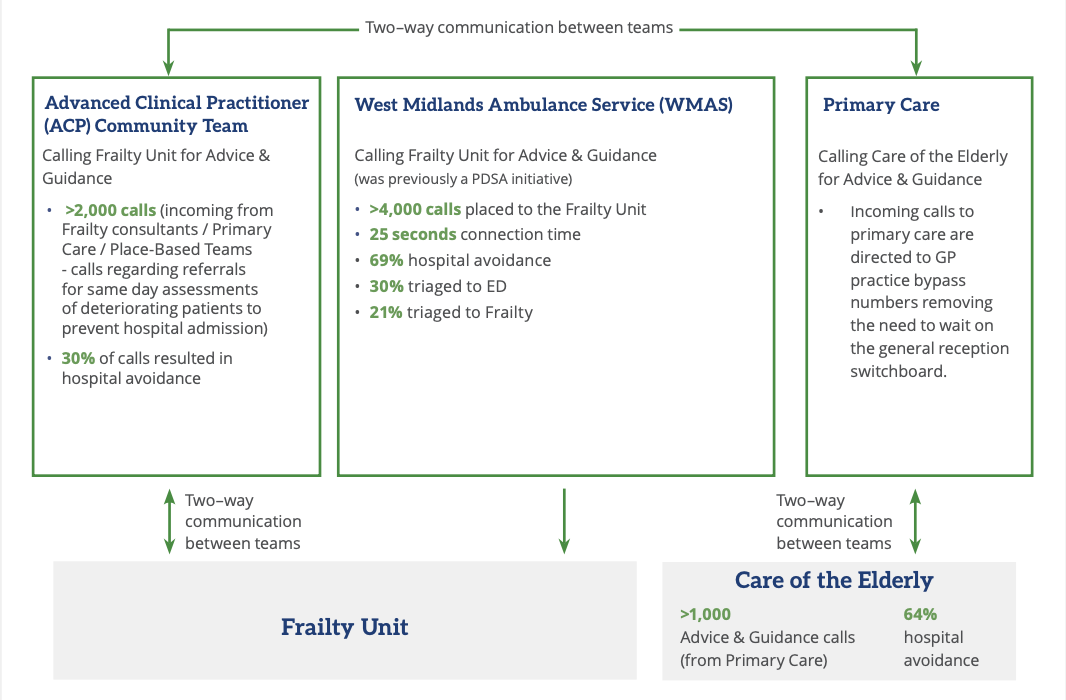
South Warwickshire NHS Foundation Trust’s (SWFT) Frailty Service has been leading an array of activities, using Consultant Connect to aid frailty patient referrals.
The diagram below illustrates how the technology is used across the trust which ultimately works towards keeping patients out of hospital where appropriate or expediting discharge. All IG-secure data, call recordings, and activity reports are available via Consultant Connect in the user’s browser for project leads to access when required.
In addition to being shortlisted for the HealthTech Partnership Award of the year, the integrated frailty service in SWFT, in partnership with Consultant Connect, recently featured in NHS England’s latest delivery plan for recovering urgent and emergency care services as an example of how to expand and better join up new types of care outside hospital.

Better visibility and improved processes for Frailty
in Buckinghamshire
Moving local hotline arrangements such as ‘on-call’ or ‘hot-week’ consultant lines to Consultant Connect brings everything in one place, centralising the whole Advice & Guidance process, delivering efficiencies, and benefiting all parties involved. This is exactly what happened to the ‘Integrated Elderly Care Silver Phone’ in Buckinghamshire Healthcare NHS Trust (BHT). Since moving the line to Consultant Connect in August 2021, the Frailty line has had over 4,700 calls placed, answered in 17 seconds on average, with 35% of calls resulted in the patient being treated out of hospital and 59% of calls resulting in patients being navigated to outpatients (e.g. MUDAS or CATS).
Silver Triage initiative helps older people living with frailty receive urgent care in their home setting
in North Central London
In 2022, the NCL Integrated Care Board (ICB) approved an initiative to set up a scheme called Silver Triage, bringing together LAS and NHS trusts. Silver Triage enables specialist geriatricians to provide advice and guidance to ambulance paramedics who are assessing older people living in care homes. The doctors can also help access and coordinate community services to provide care at home if the person does not need to go into hospital.


Consultant Connect bridges gap in frailty services
for Ambulance Trust in England
In June 2022, a pilot project was launched whereby ambulance clinicians at an Ambulance Trust in England could use Consultant Connect to seek rapid Telephone Advice & Guidance from out-of-area NHS consultants regarding frail patients, as there is no local service available.
Since the launch of the project, access to specialist advice in this way has helped avoid unnecessary patient conveyance, meaning that patients are treated in the most appropriate place for their care, and unwarranted pressures on Secondary Care are reduced, all whilst ambulance clinicians are able to receive rapid specialised advice.
Of all calls made to frailty consultants on the NCN via Consultant Connect since the set-up of this project, 88% have resulted in a patient avoiding conveyance or admission to hospital*.
Elderly Care | Patient examples
The major responsibility of looking after the healthcare needs of older patients and their families is often taken on by Primary Care professionals and Care Homes. One proven approach, being used across the UK by Primary Care and Care Homes, is Consultant Connect for rapid specialist Frailty Advice & Guidance. In many instances, an immediate verbal conversation with a Frailty specialist can render a referral unnecessary – improving patient care and providing system efficiencies.
Here are some examples of it in practice…

GP and consultant patient example
Dr Cristina Guallar, GP in Southwark and Dr Patrick Davey, Consultant Cardiologist, share how the service enabled them to provide effective cardiology care for an elderly patient:
“The patient benefited from a phone conversation with a consultant in two ways. Firstly, she was able to immediately start blood thinning treatment, which protected her against a stroke. Secondly, Dr Guallar could use my name to access early local cardiology services and assessment for aortic valve surgery, which, if possible, would dramatically improve symptoms and life expectancy. Without this phone conversation, it is likely that the referral would have been through the standard route and could have taken many months, during which time she would have been at risk of stroke and may have died from her narrowed aortic valve.” Click here to read the full case study.
GP patient example
Dr Mullin, GP in Greater Glasgow and Clyde Health Board explained how the service is useful and benefits them and their patients.
‘I saw an 88-year-old patient who was profoundly hyponatraemic which caused bradycardia and dizziness. The patient had recently undergone tests to investigate retinal artery occlusion. The urea and electrolyte results came back from the lab late in the day, but using the Consultant Connect service, I was able to speak to a consultant immediately to discuss follow-up options. The consultant advised that the patient be seen in the Department for Medicine for the Elderly the following day, where appropriate investigations could be performed, and medication reviewed. This meant that a late evening admission was avoided, and the patient’s current functional status could be discussed with the consultant who was planning the appointment.’ Click here to read the full case study.
Consultant Geriatrician patient example
Consultant Geriatrician in Sunderland, Dr Catherine Barnes explains why she likes answering Telephone Advice & Guidance calls:
The Recovery at Home Team were concerned about an elderly patient, living on her own at home. She was known to have Chronic obstructive pulmonary disease but had recently become more breathless. The patient complained of weight loss and a poor appetite and explained she had been collapsing at home. She had recently been seen in the Emergency Department, but they felt she wasn’t improving.
“We arranged an urgent Outpatient Clinic appointment, which she attended. We were able to assess her, with access to her medical records and previous investigations. Blood tests, an ECG and lying and standing Blood Pressure were checked and advice with regards to changes to her medication was given. We were able to liaise with other services involved in her care. This enabled the patient to get the assessment and support she needed without an emergency admission.” Click here to read the full case study.
Paramedic patient example
Marcus Viggers has worked as a Paramedic for the Welsh Ambulance Services NHS Trust (WAST) for nearly 20 years. He shares an example of how using the service helped avoid A&E for an elderly patient:
‘I often use Consultant Connect and I have a lot of examples where using the service has expedited my patients’ care. One involved an elderly patient with complex needs; she had multiple comorbidities, and her daughter was essentially looking after her, there was no real care package in place. I used the app to speak initially with her GP, then again to speak with one of the consultants in the local hospital. These conversations enabled us to decide that, given the patient’s history, it was best that she remained at home and was looked after from there. Being able to access multiple points of care, ensured a safe referral. We were able to improve care provision within the patient’s home and avoided an unnecessary admission. An admission would have been a disruptive and distressing for both the patient’s daughter and the patient.’ Click here to read the full case study.
A&E consultant patient example
Jonathon Will is the Clinical Effectiveness Lead, and a Specialist Paramedic & Tayside Mountain Rescue Officer at the Scottish Ambulance Service shares his experience:
One example of prof-to-prof conversations working incredibly well was a 74-year-old gentleman I attended earlier this year. He had been reported to the police as a ‘wandering dementia patient’, and when they found him, it was clear he was somewhat unstable on his feet; in fact, he already had some minor injuries consistent with a fall.
We called the prof-to-prof line and the Senior Clinical Decision Support who informed us that he had indeed been in hospital for two days being treated for acute confusion and a UTI. There were also notes to the effect that the confusion was suspected to be more chronic in nature.
On the advice of the consultant, we then contacted the patient’s own GP for a further prof-to-prof conversation. It turned out that the patient was booked for a five-day residential dementia assessment the following week.
Although we were on scene for a long time, our overall service time was not increased because we avoided a long convey and hand over at hospital. Click here to read the full case study
GP patient example
Dr Yama Rasekh is a GP at Vine House Health Centre, in the Herts Valleys CCG area and shares a recent experience:
“I saw an elderly 80-year-old patient who was waiting for a hip replacement. The operation was cancelled by the anaesthetist because the patient’s sodium level was low, and they were slightly anaemic. I carried out initial investigations, but couldn’t find a cause.
I used Telephone Advice & Guidance, via Consultant Connect, to speak to an elderly care consultant. The consultant explained that anaemia is not a contraindication, and that the patient could be transfused. I arranged further investigations for the cause of the low sodium level, or hypernatremia. I was then able to refer the patient back to orthopaedics for their operation.
Being able to get this type of advice quickly improved the care of the patient. Without the service, it may have taken three months for them to see a consultant, and by that time, the patient could have been presenting with new clinical conditions. Using the service was a good experience for myself and the patient.”
Here’s what the NHS say…
Latest news
3 ways to relieve pressures on hospital teams

Meeting the requirements of NHSE’s FRAIL strategy using Consultant Connect tech

The successful UEC pathways that are transforming the NHS through winter and beyond

Transforming the care of older people

How Consultant Connect can help implement the SAMEDAY strategy to support your SDEC pathway

Thousands of elderly patients avoid unnecessary hospital queues thanks to health tech

Using Consultant Connect for Frailty pathways

Milton Keynes Hospital celebrates first birthday of its medical centre which has treated over 20,000 patients
Contact us
For more information about how we work with commissioners, hospitals and mental health trusts to improve patient care, please get in touch.
Join a webinar
Listen to health experts from the comfort of your desk as we bring the experts to you in our series of online webinars.
Join our mailing list
Join our mailing list and we'll keep you informed of our latest blogs, project news, and upcoming webinar dates and topics.