Since the pilot project was completed, QEHKL has used Consultant Connect to triage further Cardiology referrals. Project update – in brief:
- Triaged 4,000+ Cardiology referrals since July 2021.
- 29% of referrals have been returned to the GP with detailed Advice & Guidance, which has avoided outpatient appointments. A further 25% have been booked in for diagnostics only.
This article uncovers how the pilot project was implemented and the key results.
Like many NHS areas nationwide, waiting list backlogs and staffing challenges became barriers to elective restoration work in Norfolk and Waveney. In April 2021, Queen Elizabeth Hospital King’s Lynn (QEHKL) and Norfolk and Waveney ICB decided to use Consultant Connect’s Referral Triage service to run a pilot project focussing on the first outpatient waiting list for Cardiology. This article uncovers how the pilot project was implemented and the key results.
In April 2021, Queen Elizabeth Hospital King’s Lynn (QEHKL) and Norfolk and Waveney ICB set up an initial meeting to discuss a pilot to triage 1,000 referrals using Consultant Connect’s Referral Triage service. Primary care clinicians in West Norfolk already used Consultant Connect for pre-referral Telephone Advice & Guidance (launched in October 2019).
QEHKL identified Cardiology as the specialty they wished to focus on. In mid-July 2021, Dr Stephen Cookson, NHS Cardiologist on the National Consultant Network (NCN), was instructed to work on these cardiology referrals. A comprehensive briefing with QEHKL’s clinical team took place, allowing Dr Cookson to further understand local pathways and protocols. He then triaged a small batch, which QEHKL checked to ensure consistency. Dr Cookson was subsequently given the go-ahead to triage the remaining referrals, which were completed in 7 weeks.
Outcome and Impact
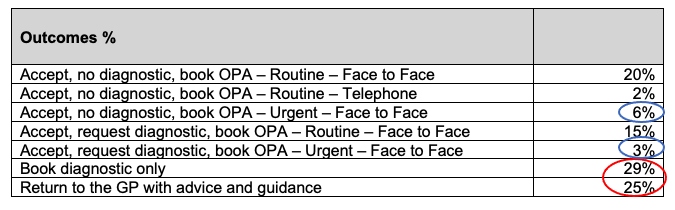
The table below shows the outcomes of the waiting list review work for 1,000 Cardiology referrals:
Reduction in first outpatient appointments
The data shows that 250 Cardiology referrals were sent back to GPs with Advice & Guidance and 29% (290) of the referrals were booked for diagnostics only. This represents a significant freeing up of outpatient capacity with over 50% of the referrals reviewed not requiring a first outpatient appointment.
Although some patients may require an outpatient appointment after having diagnostics, this will be on a more informed basis with the additional information from the investigations being available to clinicians.
As a result of this 7-week review of 1,000 Cardiology referrals, waiting times were reduced from 48 weeks to 41 weeks.
Prioritisation
This work also helped ensure that patients were seen in relation to their clinical priority rather than based only on the time they have waited. This has also enabled any Cardiology referrals that are urgent to be appropriately identified and prioritised with 9% (90 referrals) falling into this category.
This prioritisation also supports Primary Care in providing reassurance that patients have had their case reviewed and prioritised based on clinical need.
To support capacity and efficiency, the most appropriate type of appointment (face to face or telephone) is also marked against each referral. This benefits the patients who do not need to incur travel costs if a telephone consultation is deemed most appropriate.
Advice & Guidance
For the 25% of referrals returned to GPs with Advice & Guidance this was in the form of a detailed letter with information and advice about the suitable management of the patient’s condition. To support these Advice & Guidance letters a dedicated phone line (managed by Consultant Connect) was offered for referrers to ask additional questions about the information received.
Dr Steve Cookson, Consultant Cardiologist triaging the referrals comments:
‘I’m pleased that this project has brought about a reduction in waiting times when NHS services across the country are under huge pressure. I hope that facilitating investigations in advance of clinic appointments in selected cases will result in further efficiency savings, by improving the new to follow up ratio and that this free clinic capacity can be directed towards patients who need more urgent clinical review. The standard of referrals from GPs has been high, as has the IT infrastructure, meaning decisions can often be made immediately, rather than requiring back and forth messages to obtain the necessary information.’
Related materials:





